The Center’s mission is to be the world’s leader in research, education, innovation, and using information technologies to reduce medical errors, improve patient safety, and optimize patient care globally.
Based in Boston at Brigham and Women's Hospital and Harvard Medical School, the Center is a multi-institutional organization working to improve the overall quality of healthcare through scientifically proven systems, methods, and practices.
The Center is led by renowned patient safety expert, David Westfall Bates, MD, MSc, Executive Director; Gordon Schiff, MD, Associate Director; Patricia C. Dykes, RN, PhD, Program Director; and Ronen Rozenblum, PhD, MPH, Business Development Director. Center faculty members play integral roles with national regulators and government committees and have voices internationally to inform and improve patient safety standards globally.
We leverage relationships with incubators, start-up companies, and industry leaders to drive innovation in patient safety technologies while focusing on innovations to improve safety, cost effectiveness, and value.
 Brigham and Women's Hospital
Brigham and Women's Hospital
Dr. David Bates is the Medical Director of Clinical and Quality Analysis at Mass General Brigham (MGB), co-Director of the Center for Artificial Intelligence and Bioinformatics Learning Systems (CAIBILS) at MGB, and a Senior Physician at Brigham and Women’s Hospital (BWH). In June 2023, he stepped down as Chief of General Internal Medicine and Primary Care at BWH after 25 years in that role. Dr. Bates is also a Professor at both Harvard Medical School and at the Harvard T.H. Chan School of Public Health; in addition, he directs the Center for Patient Safety Research and Practice at BWH. Previously, he served as Chief Quality Officer and later as Chief Innovation Officer at BWH.
Dr. Bates is an internationally renowned expert in patient safety, using information technology to improve care, quality-of-care, cost-effectiveness, and outcomes assessment. He has served as president of the International Society for Quality in Healthcare (ISQua) and as Board Chair of the International Society of Quality and Safety.
At a time when patient safety is a key driver for focusing national attention on health-care quality, Dr. Bates' work has not only shown the magnitude of the problem but also provided a blueprint for helping to solve it. He led a seminal study on the epidemiology of drug-related injuries, demonstrating that the most effective way to prevent serious medication errors is to focus on improving the systems. He has also performed numerous studies on how computerized, evidence-based guidelines can improve quality and efficiency. Dr. Bates has been recognized for several years by Modern Healthcare magazine as one of the “100 most powerful” individuals in U.S. health care. He has published over 1,200 peer-reviewed papers which have been cited over 162,000 times; Dr. Bates is among the 400 most cited of all biomedical researchers and is listed as being among the top 500 scientists in the world.
Dr. Bates is a member of the National Academy of Medicine, the Institute of Medicine, the American Society for Clinical Investigation, the Association of American Physicians, and the American College of Medical Informatics, and was Chairman of the Board of the American Medical Informatics Association. He has also served as external program lead for research for the World Health Organization's Global Alliance for Patient Safety and is past president of the International Society for Quality in Healthcare (ISQua). In addition, Dr. Bates is the Editor of the Journal of Patient Safety.
Dr. Bates earned degrees from Stanford University (BS), the Johns Hopkins School of Medicine (MD), and Harvard T.H. Chan School of Public Health (MSc).
 Brigham and Women’s Hospital
Brigham and Women’s Hospital
Dr. Gordon (Gordy) Schiff is a practicing general internist and Associate Director of Brigham and Women’s Hospital’s (BWH) Center for Patient Safety Research and Practice, Quality Safety Director for the Harvard Medical School (HMS) Center for Primary Care and is also Associate Professor of Medicine at HMS. Prior coming to Boston in 2007, he worked for over three decades at Cook County Hospital, serving Chicago’s under-resourced patients; directing County’s General Medicine Clinic; and chairing the Quality Assurance/Improvement and Drug Formulary Committees. Dr. Schiff was also a Professor of Medicine at Rush Medical College.
Dr. Schiff has published more than 250 articles and chapters on patient safety and quality, particularly in the areas of medication and diagnosis safety (including the Harrison’s Textbook of Medicine Chapter on Improving Diagnosis). He was a reviewer and contributor to the 2015 National Academy of Medicine Report, Improving Diagnosis in Health Care, and is a founding member of the Society for Improving Diagnosis in Medicine (SIDM).
Dr. Schiff has been PI on multiple AHRQ, CRICO, NSPF, and Gordon and Betty Moore Foundation-funded projects related to improving medication safety and application of health IT to safer medication use. He is currently PI on an AHRQ Diagnostic Center for Excellence (Improving Cancer Diagnosis (ICDx) which focuses on learning from and supporting patients with potentially delayed cancer diagnosis; this involves linking CRP (Communication and Resolution Programs) with diagnosis improvement. In addition, Dr. Schiff is the course director of the Harvard Master’s in Quality in Safety Special Topics Course.
Dr. Schiff won an award from the Arnold Gold Foundation for Medical Humanism to study clinician-patent boundaries. He was recipient of the 2019 Mark Graber Diagnosis Safety Award from SIDM, the 2020 Eisenberg Award by the National Quality Forum (NQF) and the Joint Commission, and 2021 Avedis Donabedian Quality Award from the American Public Health Association (APHA). He currently chairs the editorial board of Medical Care and serves on the editorial boards of the Journal Public Health Policy and BMJ Quality and Safety in Healthcare. He is a founding member of Physicians for a National Health Program (PNHP).
Dr. Schiff is a graduate of Rush Medical College of Rush University and Tufts University.
 Brigham and Women’s Hospital
Brigham and Women’s Hospital
Dr. Patricia Dykes is a Professor of Medicine at Harvard Medical School and the Research Program Director for the Center for Patient Safety, Research and Practice at Brigham and Women’s Hospital in Boston (BWH). She has conducted extensive research in the field of informatics and patient safety, focusing on leveraging information technology to enhance patient safety outcomes. Dr. Dykes' research encompasses the development and implementation of various informatics interventions, including clinical decision support systems aimed at reducing patient falls, pressure injuries, diagnostic errors, improving communication among healthcare providers, and preventing adverse events.
Dr. Dykes has performed research focused on patient fall prevention. With Robert Wood Johnson Foundation funding, she developed the Fall (TIPS) Tailoring Interventions for Patient Safety program, obtained stakeholder input for development/validation of necessary tools and software, conducted a randomized trial, and demonstrated a 25% reduction in hospitalized patients’ falls. In a subsequent AHRQ-funded study, Dr. Dykes and her team found that a refined “patient centered” Fall TIPS program produced a 34% reduction in injurious falls. Using EHR data from two large and diverse health systems (the dataset included over 900,000 patients and over 10,000 falls) to investigate the costs of inpatient falls and the cost savings associated with implementation of the Fall TIPS program, they found that the total average cost of a fall was $62 521 and that the costs of falls only differed marginally by injury level. They found that implementation of the evidence-based Fall TIPS program was cost effective and was associated with lower inpatient cost and care burdens.
Dr. Dykes authored two books and over 190 peer reviewed publications and has presented her work nationally and internationally. She is past President and Board Chair of the American Medical Informatics Association, formerly served on the Nursing Informatics Task Force and Committee Chairs for the Health Information Managements and Systems Society and was a founding Governing Director for the Alliance for Nursing Informatics. Dr. Dykes is a current board member of the National Pressure Injury Advisory Panel, an elected fellow of American Academy of Nursing, the American College of Medical Informatics, and the International Academy of Health Sciences Informatics.
Dr. Dykes’ impact in promoting safe patient care has been widely recognized by others in the patient safety and informatics communities in the United States and globally. She is a frequent speaker on patient safety topics and has delivered numerous local, regional, national, and international presentations to disseminate her work.
Dr. Dykes earned her BS in Nursing from Fairfield University, a Master’s in Nursing from New York University, and a Doctorate in Nursing Informatics from Columbia University.
 Brigham and Women's Hospital
Brigham and Women's Hospital
Dr. Ronen Rozenblum is a healthcare executive, researcher, lecturer, and entrepreneur, and an Assistant Professor at Harvard Medical School (HMS), in addition to his role with the Center. He is an expert and international leader in patient-centered care, patient experience, patient engagement, and health information technology. Dr. Rozenblum’s research, lectures, and contributions in these domains have been recognized nationally and internationally.
Dr. Rozenblum established, developed, and is now the Director of the Unit for Innovative Healthcare Practice and Technology at Brigham and Women’s Hospital. The unit’s mission is to establish and support a structured, long-term relationship between the Center of Patient Safety Research and Practice and industry through scientifically proven digital and information systems, methods, and practices.
Dr. Rozenblum has led and been involved in several research projects and quality improvement initiatives around patient-centered care and health information technology. He has a breadth of expertise and practical knowledge in developing and implementing innovative methods and information technologies to enhance patient-centered care, patient experience, and patient engagement. He has trained many clinicians to implement these tools in clinical settings and has presented his work at several national and international conferences. As well, Dr. Rozenblum is involved in numerous teaching and mentoring activities at HMS and Harvard T.H. Chan School of Public Health. He has also published several papers related to patient-centered care, experience, and engagement, and co-edited a pioneering book on health information technology and patient empowerment, “Information Technology for Patient Empowerment in Healthcare.”
Dr. Rozenblum was appointed as an International Expert at the International Society of Quality in Healthcare (ISQua) and elected as a lifetime member of the Academy of Quality and Safety in Health Care (IAQS) to recognize his contributions to the field of Healthcare Quality and Safety globally. He co-leads the development of patient-centered care criteria for the Adult Congenital Heart Disease Program Accreditation in the U.S. and was a member of the U.S. Government Accountability Office Expert Group working on Artificial Intelligence (AI) in Health Care, reporting to the U.S. Congress. Internationally, Dr. Rozenblum was a member of the World Health Organization Global Expert Consultation group, which worked to establish an international framework for patient and family engagement. In addition, he is a member of the Steering Committee evaluating the national rollout of the National Health Service (NHS) App in England and has been involved in several activities to promote patient-centered care in Israel with the Israeli Ministry of Health.
As well as the aforementioned work, Dr. Rozenblum works in establishing and managing startup companies in the healthcare industry, with experience in business development, marketing, and management. He holds an MPH and a PhD in Business Administration, Health Management and Economics. He completed his post-doctoral research fellowship in patient-centered care, patient experience and engagement, and medical informatics at Harvard Medical School.
Dr. David Feygin is the CEO and Co-Founder of Redesign Health, a company that powers innovation in healthcare by developing technologies, tools, and insights that lowers barriers to change across the industry. Since 2018, exceptional founders have built over 50 companies at Redesign, impacting more than 10 million lives across many aspects of the healthcare ecosystem, including cancer care, teleaudiology, COVID-19 testing, and metabolic health.
In 2022, Dr. Feygin founded ANAVO DX, which accelerates the Digital Health development lifecycle and empowers companies to bring lifesaving and life-improving digital innovation to patients and doctors. He is a member of the Board.
As Chief Digital Health Officer at Boston Scientific for many years, Dr. Feygin led the company’s Digital Health strategy and was responsible for leading the core Big Data, Internet of Things (IoT), Analytics and Mobility teams, and partnering to establish the evolving capabilities that to ensure enterprise success in Digital Health. He also chaired the cross-functional Digital Health Council.
Prior to Boston Scientific, Dr. Feygin was Vice President of Corporate Strategic Innovation for Becton Dickinson (BD), responsible for integrating company-wide activities focused on identifying new market opportunities outside existing core areas and developing high-impact growth concepts that fall outside of, or cut across, existing business units. As Worldwide Director of Strategic Innovation for the BD – Medical Surgical Systems (MSS) business unit, he developed and led the MSS Strategic Innovation Group, which was responsible for identifying, developing, and validating opportunities and overall growth strategies. The Strategic Innovation Group was also responsible for strategic marketing, market analytics, opportunity sensing, sourcing and evaluation, health economics analysis, fundamental business analytics, advanced customer research, and driving innovation initiatives from market, clinical, technical, and policy perspectives.
Dr. Feygin earned a Bachelor of Engineering at The Cooper Union and a PhD in Mechanical Engineering from the University of California, Berkeley for his work in virtual environments and medical simulation. He spent four years at medical simulator startups leading the development, commercialization and launch of state-of-the-art simulators including the Virtual I.V. ™ product line. As well, Dr. Feygin earned an MBA from the Harvard Business School.
Mr. Geoff Fiedler is responsible for setting the corporate vision and strategy for Aceso® and oversees all of the company’s business development, sales, and marketing activities. Over the course of more than 20 years in the healthcare industry, Mr. Fiedler has established many long-term strategic relationships throughout the healthcare industry.
Mr. Fiedler’s career is highlighted by a range of entrepreneurial experiences across different industry sectors with a focus on healthcare and patient and family engagement/experience. He co-founded Innovative Medical Solutions, the predecessor to Aceso, in 2007. Prior to that, he spent nearly a decade in sales, consulting, marketing, and business development with Cerner Corporation. During his tenure at Cerner, Mr. Fiedler pioneered several strategic initiatives focused on interoperability and streamlining the patient/physician relationship.
Prior to Cerner, Mr. Fiedler held several senior executive level positions with various national corporations and associations. He is a graduate of the University of New Hampshire with a BS degree in Kinesiology.
Carol Keohane has been the Senior Vice President and Chief Quality and Patient Safety Officer at South Shore Health since 2022. Prior to that, she was the Vice President, Quality, Safety, Experience and Health Systems Performance Improvement at Kaiser Permanente, where she led improvement system design, build capacity, and partner with teams across the organization, linking strategy to execution to optimize national outcomes in quality, safety, experience, performance improvement, care delivery redesign, and management. In addition, she provided leadership for 90 team members with an extensive portfolio of quality, safety, care experience, and performance improvement initiatives.
Ms. Keohane is a value-driven and mission-centric healthcare executive with a dynamic background and strong expertise in driving successful and cost-effective healthcare delivery programs. She has a proven track record of delivering innovative solutions and results in the areas of quality, safety, risk, regulatory, accreditation, clinical operations, women’s and children’s health, and patient experience. In addition, she is a recognized and compassionate thought leader with an unwavering commitment to building national clinical programs that transform patient care delivery and outcomes.
Before joining K-P, Ms. Keohane spent several years at CRICO/Risk Management Foundation (of Harvard’s Medical Institutions), with responsibility for the strategic direction, programmatic development, daily operations, and financial management of CRICO/RMF's Patient Safety Division. Prior to CRICO, she was a nurse first at Beth Israel Deaconess Medical Center and later at Brigham and Women’s Hospital. She earned her BSN in Nursing at Saint Anselm College and her MS in Health Informatics and Management at UMass Lowell.
David Kronfeld is an experienced venture capital investor and telecommunications industry executive with over 40 years of experience. He founded JK&B Capital in 1996 and prior to that, was a general partner at Boston Capital Ventures (BCV), where he focused on making venture capital investments in companies within the communications and software industries.
Before joining BCV, Mr. Kronfeld was the vice president of acquisitions and venture investments at Ameritech, responsible for directing Ameritech’s venture capital investments and all of the company’s mergers and acquisitions activities. In addition, he was a senior manager at Booz Allen and a systems analyst at Electronic Data Systems (EDS). Mr. Kronfeld earned a BS degree in Electrical Engineering with high honors and an MS in Computer Science from Stevens Institute of Technology, as well as an MBA from The Wharton School of Business at the University of Pennsylvania.
 Press Ganey
Press Ganey
Dr. Thomas Lee is an internist practicing at Brigham and Women’s Hospital in Boston, MA, and the Chief Medical Officer of Press Ganey, Inc. Prior to joining Press Ganey in 2013, Dr. Lee was Network President for Partners Healthcare System (now Mass General Brigham), the integrated delivery system founded by Brigham and Women’s and Massachusetts General Hospitals.
Dr. Lee has performed research leading to more than 300 articles in peer-reviewed journals and five books; he was most recently published in Healthcare’s Path Forward (2023). He is also a Professor at both Harvard Medical School and Harvard School of Public Health. In addition, Dr. Lee is Editor-in-Chief of NEJM Catalyst and a member of the Editorial Board of The New England Journal of Medicine, the Board of Directors of Geisinger Health System, the Board of Directors of Blue Cross Blue Shield of Massachusetts, the Board of Directors of Health Leads, and is on the Panel of Health Advisors of the Congressional Budget Office.
Dr. Lee earned his BA from Harvard College and his MD from Cornell University Medical College, and then trained in internal medicine and then cardiology at Brigham and Women’s Hospital. He then earned a MSc in Epidemiology from Harvard School of Public Health.
 Nurse Executive and Health IT Leader
Nurse Executive and Health IT Leader
Judy Murphy is a nurse executive and health IT leader with a long history in health informatics. She was Chief Nursing Officer (CNO) at IBM Global Healthcare, where she built relationships, expanded business across the healthcare industry, and served as strategic advisor to clients. She was a member of the IBM Industry Academy and a much sought-after consultant and speaker on the digital transformation of healthcare. Her expertise lies in advancing tools for consumer engagement, provider enablement, and analytics for population health management; using cognitive computing to support a Learning Healthcare System; as well as promoting the use of mobile to streamline clinical workflow and create the care team of the future. Ms. Murphy has a long-standing reputation of patient advocacy and maintaining a “patient-centric” point of view, approaching her work with unyielding energy and passion and commitment to technology-enabled healthcare transformation.
Prior to working at IBM, Ms. Murphy was CNO and Deputy National Coordinator for Programs and Policy at the Office of the National Coordinator for Health IT (ONC) in Washington DC. In these roles, she led federal efforts to assist healthcare providers in adopting health information technology to improve care and to promote consumers’ greater understanding and use of health information technology. While at the ONC, she participated on the National Committee on Vital and Health Statistics (NCVHS), the Health IT Policy Committee, and the Health IT Standards Committee.
Ms. Murphy has over 25 years of health informatics experience at Aurora Health Care in Wisconsin. As Vice President-EHR Applications, she led their EHR program since 1995, when Aurora was one of the early adopters of health IT, and helped it earn Hospital & Health Networks' "100 Most Wired" award for eight years. While there, Ms. Murphy served on the Health IT Standards Federal Advisory Committee since it began in 2009, and both co-chaired the Implementation Workgroup and was a member of the Meaningful Use Workgroup.
Ms. Murphy’s work has been recognized with Fellowship in the American Academy of Nursing (AAN) and the American College of Medical Informatics (ACMI). In 2022, she received an honorary Doctor of Nursing degree from the University of Wisconsin-Milwaukee and in 2018, was awarded Lifetime Fellowship in HIMSS. She has received numerous significant awards throughout her impressive career. In 2007, Ms. Murphy was named one of the “20 People Who Make Healthcare Better” by HealthLeaders magazine and was chosen as one of 33 Nursing Informatics’ Pioneers showcased in the Nursing Informatics History Project sponsored by AMIA, NLM, AAN, and RWJF.
Ms. Murphy is a tireless volunteer who has been involved in many aspects of organizational work throughout her career. Within HIMSS, she served in several capacities, including serving on the Board of Directors. Since its inception in 2007, Ms. Murphy was a member of the Alliance for Nursing Informatics (ANI) and served as its Co-Chair for six years. In addition, she was of the original American Association of Medical Informatics (AMIA) members and served on numerous committees, task forces, and the Board of Directors.
Tim O'Malley started his career at Siemens Medical Systems, where he spent 16 years. While there, he built the Electromedical businesses (Cardiology, Life Support Systems, Patient Monitoring) to become Siemens’ second largest medical division in the US. He also held positions in Technical Support Services, Marketing and Product Management, Sales, and General Management.
Mr. O’Malley has had the privilege of working with innovative technologies, all dedicated to helping clinicians improve patient care. In other med tech positions, was CEO of Medwave, Inc., an innovative public company that developed sensor-based Continual Non Invasive Blood Pressure technology.
In 2007, Mr. O’Malley joined ZOLL Medical to lead its Hospital Division; he was recruited to drive market adoption and business growth. ZOLL had previously introduced an innovative Defibrillation (Cardiac Resuscitation) Platform in the R-Series. At the end of his 5-year stint there, the hospital business went from approximately 35% to over 60% market share.
Throughout his career, Mr. O’Malley has worked with clinicians and healthcare systems to develop intersections of care between patients, caregivers, and technology which, when applied through proper process management, has proven to produce incredible results in patient care, outcome improvements, patient well-being, and favorable cost positions.
Mr. O’Malley was President and Chief Growth Officer of EarlySense, Inc., from 2012 until 2020. While there, he steered the company into commercializing the innovative EarlySense Sensor based, Contact Free Patient Monitoring System. The results were agreements with Bose, Google, Herman Miller, Welch Allyn, and Hill-Rom, which acquired EarlySense’s Hospital Business in early 2021.
Currently, Mr. O’Malley is Vice President and Division Manager of Healthcare at TPC Systems, a 90-year-old family business. He is responsible for managing the current product portfolio, as well as bringing on new and innovative products. These products encompass Fall Prevention Technology, RTLS Platforms, Clinical Communications, Data, Analytics and Alarm Management Systems, and Infant Security products. Mr. O’Malley has had several US patents listed, including patents for Data Transfer and Downloading, Assessing Cardiac Function from a wrist sensor, and Using Past Cardiac Performance to assess future performance expectations.
Dr. Roy Schoenberg is Amwell's President and Chief Executive Officer. Since co-founding the company with his brother, Ido, in 2006 and taking it public in 2021, Amwell has become one of the world’s largest digital networks, helping patients, clinicians, and payers welcome a new world of tech-enabled healthcare.
Prior to founding Amwell, Dr. Schoenberg was founded CareKey and was Chief Information Security Officer at TriZetto, following its acquisition of CareKey. In 2013, he was appointed to the Federation of State Medical Boards’ Taskforce that issued the landmark guidelines for the “Appropriate Use of Telemedicine in the Practice of Medicine”. In 2020, Dr. Schoenberg was named one of Modern Healthcare’s 100 Most Influential People in Healthcare and was the 2014 recipient of the American Telemedicine Association Industry award for leadership in the field of telemedicine.
Outside of Amwell, Dr. Schoenberg is on the advisory board of the MIT Sloan Health Initiative and the American Heart Association Telehealth board; Modern Healthcare has repeatedly recognized him as one of the 100 Most Influential People in Healthcare. He is a former American Telemedicine Association board member, and that organization has recognized him for his industry leadership. Dr. Schoenberg continues to see innovation in digital care as his calling, holding more than 50 US-issued patents in this domain.
Dr. Schoenberg earned an MD from The Hebrew University and an MPH from Harvard T.H. Chan School of Public Health.
Becton Dickinson
Dr. Joseph Smith is Senior Vice President and the Chief Science Officer at Becton, Dickinson. In that role, he is responsible for external innovation and BD’s technology roadmap to deliver transformative innovations that aligns with smart connected care, the transition to new care settings, and chronic disease. In addition, he is an Adjust Associate Professor in and an advisory board member to the Department of Biomedical Engineering at Johns Hopkins University.
Prior to working at BD, Dr. Smith was president and CEO of Digital Health Corporation with responsibility for the company’s strategy to invest in or acquire digital health and therapeutic technologies. In addition, he has held medical, scientific, and technology leadership positions at organizations including Johnson & Johnson, Boston Scientific, and the West Health Institute. He also served on the faculty at Washington University School of Medicine and Department of Biomedical Engineering.
Dr. Smith earned a bachelor's degree in electrical and biomedical engineering from the Johns Hopkins University; a master's degree in electrical engineering from the Massachusetts Institute of Technology; a PhD in medical engineering and medical physics from the Harvard/MIT Division of Health Sciences and Technology; and an MD from Harvard Medical School. He performed his internship, residency, and fellowship at Brigham and Women’s Hospital.
Dr. Paul Varghese is Head of Health Informatics for Verily (Google Life Sciences). A cardiologist and clinical informatician, Dr. Varghese helps lead Verily's efforts in the application of advanced data science methodologies to improve patient outcomes and patient-provider interactions. Before joining Verily, Dr. Varghese was Medical Director for Cardiovascular IT at Agfa Healthcare and was responsible for product design, interoperability, and quality/regulatory affairs. He currently serves on the American College of Cardiology Innovation Advisory Group.
Dr. Varghese holds a ScB and MD from Brown University, and a MMSc in biomedical informatics from Harvard Medical School. He did his internal medicine residency training on the Osler Medical Service at Johns Hopkins Hospital, a cardiology fellowship at UCSF, where he specialized in heart failure and echocardiography, and performed quality improvement/patient safety training at Intermountain Healthcare's Advanced Training Program.
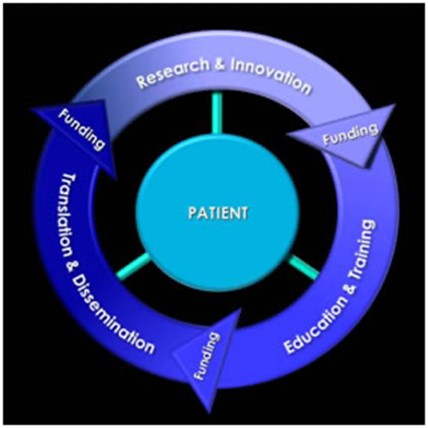
Four major areas comprise the strategic plan for the Center:
The following diagram shows the interdependence of each of those strategic areas with funding as an accelerator to the success of each initiative.
For over a century, a leader in patient care, medical education and research, with expertise in virtually every specialty of medicine and surgery.
About BWH