Discussion with Antonio Chiocca, MD, PhD, Director of Surgical Oncology, Center for Neuro-oncology, Mass General Brigham.
A: Glioblastoma, unlike other cancers, remains localized in the brain without metastasizing. However, it poses a unique challenge as it tends to recur persistently.
A: Interestingly, traditional risk factors like sun exposure, smoking, or drinking aren't associated with glioblastoma. However, exposure to radiation in early life, such as in the aftermath of events like the Chernobyl nuclear accident, has been linked to its development.
A: Genetically engineered oncolytic viruses were developed almost 20 years ago but took time to translate into patient treatments. Our approach involves injecting these viruses directly into the tumor, where they activate the immune system to attack the cancer cells. Unlike traditional treatments, our research focuses on changing the tumor microenvironment to make it less hospitable to cancer growth.
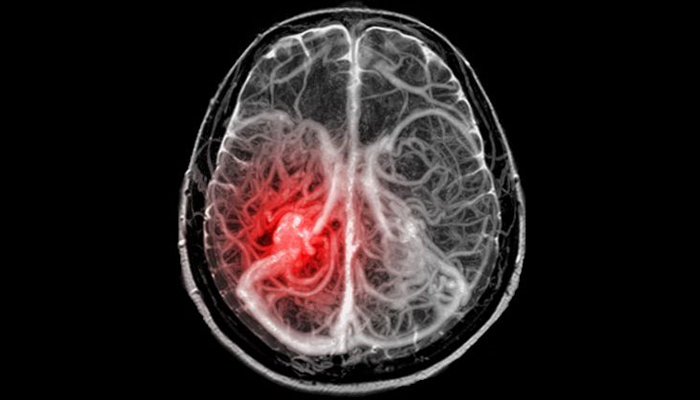
A: Glioblastoma poses a challenge to therapies, particularly immunotherapies, due to its ability to evade immune responses. Oncolytic viruses are injected directly into the tumor, where they target and reshape the tumor's supporting cells, making them more anti-tumor and less supportive of cancer growth.
A: Glioblastoma is often termed an "immune desert" due to its lack of anti-tumor immune cells. Virotherapy aims to change this by activating the immune response within the tumor, turning it into an environment that fosters anti-tumor activity. This shift enhances the body's ability to recognize and combat the tumor. Think of it this way: the tumor is a thief that broke into your home and think of the T-Cells (immune cells) as the police. The thief has turned off the alarm system so the police doesn’t know that there’s a thief inside your house. The oncolytic virus is your friendly neighbor that sees the thief and calls the police so they can come and take the thief away.
A: Genetically engineered oncolytic viruses specifically target tumor cells while sparing healthy ones, offering a more targeted approach compared to traditional treatments like chemotherapy. This targeted approach minimizes side effects and offers the potential for more effective treatment of glioblastoma tumors.
A: Early results from our clinical trials show promising outcomes. In one trial involving recurrent glioblastoma patients, we observed a doubling of median survival time, from around 6-7 months to about 14 months. While this may not seem like a significant increase, doubling survival in recurrent glioblastoma is a noteworthy achievement.
A: The Dana-Farber Brigham Cancer Center's collaborative infrastructure allows for the translation of laboratory findings into innovative patient treatments. Patients come to us from around the world for access to cutting-edge treatments not available elsewhere. And you can see the passion of its staff, not just the doctors, but also the clinical research coordinators, the scientists, and the fellows, on the work we’re doing.
A: Currently, the treatment is in clinical trial stages and showing promise. Once we complete our ongoing trials, the next step is to conduct larger trials to demonstrate effectiveness and obtain FDA approval. Patients eligible for these trials typically have recurrent tumors and must meet specific criteria for treatment. We are also currently working on another study that involves multiple injections over time and getting multiple biopsies that help us see changes in the tumor.
A: By demonstrating the ability to modify the immune microenvironment within glioblastoma tumors, this research opens doors to potential combination therapies that could enhance existing treatments. The specificity of oncolytic viruses offers hope for more effective and targeted treatments.
For over a century, a leader in patient care, medical education and research, with expertise in virtually every specialty of medicine and surgery.
About BWH