One of the leading gynecologic cancers among women, ovarian cancer is a significant diagnosis often caught at later stages. Taymaa May, MD, MSc, Director of Ovarian Cancer Surgery at Dana-Farber Brigham Cancer Center, answers some common and often misunderstood questions about ovarian cancer, and shares with us what advances Dana-Farber Brigham Cancer Center is making in the treatment of this disease.
A: Ovarian cancer affects about 1.5% of the population, making it the second most common gynecologic cancer. However, it is the leading cause of death from gynecologic tumors. It’s called the “silent killer” because it often presents without clear or alarming symptoms. Patients typically don’t experience significant pain or bleeding. Instead, they have vague symptoms like abdominal distension (bloating), mild nausea, changes in bowel habits, decreased appetite, and feeling full quickly. These symptoms are gradual and nonspecific, and don’t cause significant concern to urgently see a doctor. When patients seek medical attention, they sometimes undergo gastrointestinal workups before undergoing gynecologic workup. Ovarian cancer is usually only diagnosed through imaging tests and often diagnosed when it has already reached an advanced stage. About 70% of cases are diagnosed at this late stage.
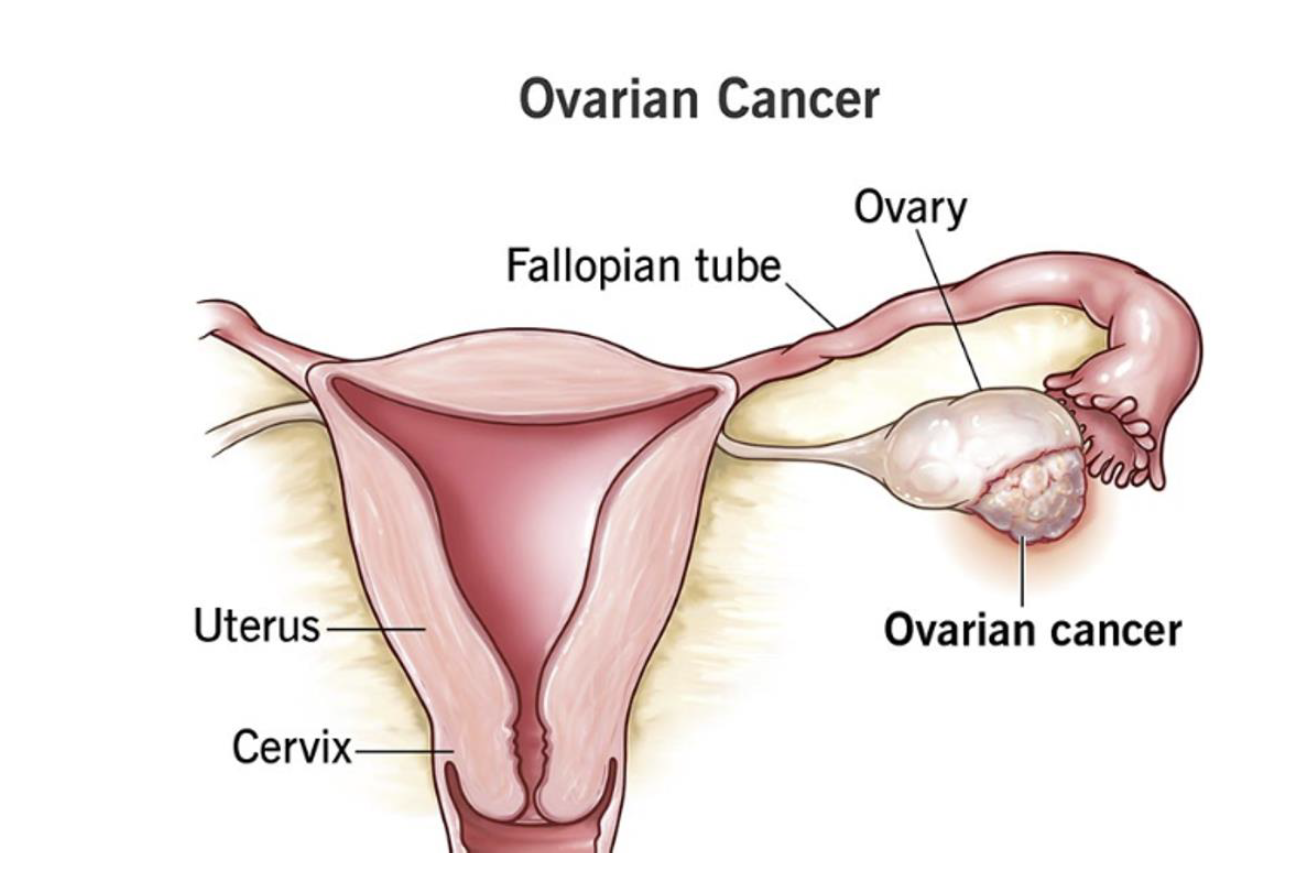
A: The most common type of ovarian cancer is epithelial ovarian cancer, which originates in the fallopian tubes and the surface of the ovary. This type primarily affects women after menopause, typically in their late 50s, 60s, or 70s. While there are rare types of ovarian cancer that can occur in younger individuals, the general risk increases with age.
A: Unfortunately, there is currently no screening test for ovarian cancer. A Pap smear screens for cervical cancer, not ovarian cancer. Several studies have tried to use ultrasound or tumor markers in the blood, but none have been successful. To date, no effective screening method for early detection of ovarian cancer has been found.
A: Many studies are looking into different markers, such as blood tests or liquid biopsies, to identify ovarian cancer earlier. Education is crucial, and patients and healthcare providers need to be aware of the common symptoms of ovarian cancer and that if someone is experiencing symptoms concerning for ovarian cancer like bloating or changes in bowel habits, it’s important to have ovarian cancer in the differential diagnosis and do the relevant investigations to rule it out.
A: Yes, BRCA1 and BRCA2 mutations increase the risk of both breast and ovarian cancer. Women with these mutations are recommended to undergo earlier screening and —after completing childbearing— prophylactic surgery to remove the fallopian tubes and ovaries to reduce their risk of ovarian cancer. At Dana-Farber Brigham, we have special clinics that monitor and follow patients with these mutations. Other genetic mutations can also increase the risk of ovarian cancer, and genetic testing is available to family members who may also be at risk.
Learn more about the BRCA test.
A: If a family member is diagnosed with ovarian cancer, genetic testing is usually performed on the patient first. If they test negative, the family’s risk remains the same as the general population. If they test positive for a mutation, the genetic counselors will determine which other family members should be tested based on their relationship to the patient.
A: The traditional form of tubal ligation, which involved clipping the tubes, is no longer recommended. We now recommend removing the fallopian tubes completely when a patient is seeking tubal ligation. This has been shown to decrease the risk of ovarian cancer. Research has found that what we often call “ovarian cancer” frequently originates in the fallopian tubes and removing them reduces the risk.
A: We’re making great strides at Dana-Farber Brigham. On the surgical side, we’re using new technologies and innovations that aid in surgical precision and improve recovery. We have several surgical trials including a study investigating the role of minimally invasive surgery in patients with ovarian cancer. Our medical oncologists are conducting clinical trials to identify the best treatments, including targeted therapies. We also perform genomic testing to understand the biology of each patient’s tumor, which allows us to personalize treatments and improve outcomes.
A: Most people are diagnosed at an advanced stage, which is treated with a combination of surgery, chemotherapy, and sometimes targeted therapy. Surgery can be performed upfront for eligible patients, followed by chemotherapy. Alternatively, neoadjuvant chemotherapy can be prescribed upfront followed by interval surgery. Chemotherapy can be administered intravenously or directly into the abdominal cavity (intraperitoneal). In some cases, hyperthermic (heated) intraperitoneal chemotherapy (HIPEC) is used during surgery, where chemotherapy is applied directly to the abdomen after the tumor is removed. Our personalized treatment approach allows for comprehensive therapeutic options that improve survival.
A: Ovarian cancer is a serious diagnosis, but there’s a lot of research and clinical advancements being made to improve outcomes. We treat ovarian cancer using a multidisciplinary approach, meaning we work as a team of oncologists, surgeons, nurses, and other specialists to tailor treatment for each patient. Our team is dedicated to supporting patients and their families throughout their journey, from diagnosis to treatment and survivorship. We’re here to help and will always do our best for our patients.
Take the ovarian cancer risk assessment.
For over a century, a leader in patient care, medical education and research, with expertise in virtually every specialty of medicine and surgery.
About BWH